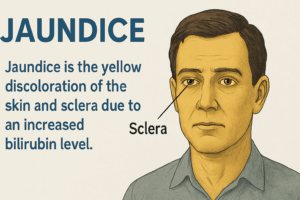
JAUNDICE
Jaundice is the yellow discoloration of the sclera, skin and mucous membrane resulting from an increased bilirubin concentration in the body fluid (more than 3mg dl). In Jaundice Type, Mechanism, Evaluation, and Examination, we will explain why it is an important topic for examination, as patients may present with acute or chronic liver disease, congenital hyperbilirubinemia, hemolytic anemia, or recurrent jaundice.
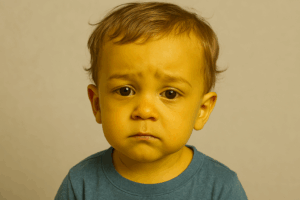
Jaundice is a condition where the skin, eyes, and mucous membranes turn yellow. This happens because bilirubin levels in the body rise above normal. Usually, bilirubin is processed by the liver and removed. But when something disrupts this process, it accumulates in the blood and causes jaundice.
There are many reasons why jaundice occurs. Some people have liver diseases, while others have blood disorders that lead to excessive red blood cell breakdown. Sometimes, it’s due to inherited conditions. Whatever the cause, jaundice is a sign that something is wrong inside the body and needs attention.
The process of jaundice begins in different ways. Sometimes, bilirubin production increases too much, overwhelming the liver. Other times, the liver struggles to absorb it properly. In certain cases, the enzymes needed to process bilirubin are missing or defective. Another cause is bile flow obstruction, preventing bilirubin from leaving the body.
Jaundice comes in different forms. Hemolytic jaundice is caused by excessive red blood cell destruction. Congenital hyperbilirubinemia happens due to genetic conditions. Cholestatic jaundice occurs when bile flow is blocked, either inside or outside the liver.
Symptoms vary depending on the cause. Some patients experience mild jaundice, while others develop severe complications. Dark urine, pale stools, and liver enlargement may be present. Fever, itching, and weight loss can also occur, especially in cases of obstructive jaundice.
Jaundice involves careful examination, history-taking, and laboratory tests. Doctors check bilirubin levels to determine whether the problem is in the liver, blood, or bile ducts. Early diagnosis is crucial for proper treatment and management.
MECHANISM OF JAUNDICE PRODUCTION
Bilirubin buildup in the blood happens in four ways. First, overproduction can overload the liver. This often occurs in hemolytic conditions where red blood cells break down too quickly, producing excessive bilirubin.
Second, problems with hepatic uptake can prevent bilirubin from entering liver cells effectively. Normally, bilirubin moves from blood into liver cells for processing. However, disruptions in this transport system block its movement, leading to accumulation.
Third, reduced conjugation can interfere with bilirubin processing inside liver cells. Enzymes play a crucial role in modifying bilirubin, making it easier to excrete. If these enzymes are missing or defective, bilirubin remains unprocessed and builds up in the bloodstream.
Lastly, issues with excretion lead to bilirubin retention. This can happen due to liver dysfunction or bile duct obstruction. When bile flow is blocked inside the liver, it’s called intrahepatic cholestasis. Viral infections or certain drugs can cause this condition. In contrast, extrahepatic cholestasis occurs when something physically obstructs the bile ducts outside the liver, like gallstones or pancreatic tumors.
Each of these mechanisms affects how bilirubin circulates in the body. A healthy liver processes and removes bilirubin efficiently. But when any step in this system fails, bilirubin accumulates, causing jaundice. Identifying the underlying cause is crucial for treatment, as different conditions require different approaches. Whether it’s excessive production, transport issues, enzyme deficiencies, or bile duct obstructions, understanding the mechanism helps guide medical decisions.
TYPES
1. Hemolytic jaundice
2. Congenital hyperbilirubinemia
3. Cholestatic jaundice may be intrahepatic or extrahepatic.
HEMOLYTIC JAUNDICE
Hemolytic jaundice happens when red blood cells break down too fast, releasing excess bilirubin into the bloodstream. The liver usually processes bilirubin efficiently, but when red cell destruction speeds up, bilirubin production overwhelms the liver’s ability to clear it. As a result, the skin and eyes develop a yellowish tint.
Etiology
There are two main causes of hemolytic jaundice: external factors affecting red blood cells and internal defects within the cells themselves.
Extra-Erythrocytic Abnormalities
Several external conditions can trigger excessive red blood cell breakdown. Malaria, a parasitic infection, destroys red blood cells and raises bilirubin levels. Autoimmune diseases cause the body’s defense system to attack its own cells, leading to early destruction. Physical trauma, such as burns or prosthetic heart valves, also damages red blood cells. Chemical exposure, especially certain medications like dapsone, can worsen the condition. Metabolic disorders, such as uremia, interfere with normal red blood cell function, further increasing bilirubin levels.
Intra-Erythrocytic Defects
Certain inherited conditions directly affect red blood cells. Spherocytosis and thalassemia make cells fragile, causing them to break down prematurely. Enzyme deficiencies, including glucose-6-phosphate dehydrogenase deficiency, weaken cell membranes. Lack of essential nutrients, such as vitamin B12 and folic acid, disrupts proper red blood cell production, increasing their destruction rate.
Clinical Features
Symptoms of hemolytic jaundice vary depending on the severity of red blood cell breakdown. Fortunately, a healthy liver can process bilirubin up to six times its normal capacity, which keeps the condition mild in many cases.
Jaundice appears as mild yellowing of the skin and eyes.
Pallor develops due to anemia caused by excessive red blood cell destruction.
Splenomegaly, or an enlarged spleen, occurs because the organ works harder to remove damaged red blood cells.
Dark-colored stool results from excess stercobilinogen, a bilirubin byproduct.
Dark urine appears due to increased urobilinogen levels.
Investigations
Doctors use various tests to diagnose hemolytic jaundice.
Liver Function Tests (LFTs): Plasma unconjugated bilirubin is elevated but usually remains below 6 mg/dL. Liver enzymes and albumin levels stay within the normal range, confirming that liver function is preserved.
Urine Analysis (D/R): No bilirubin appears in the urine since the excess bilirubin is unconjugated and not water-soluble. However, urinary urobilinogen levels are raised, reflecting increased bilirubin metabolism.
CHOLESTATIC JAUNDICE
Cholestatic jaundice occurs when bile flow is obstructed, preventing bilirubin from being properly excreted. This leads to a buildup in the blood, causing yellow discoloration of the skin and eyes. The obstruction can occur inside the liver (intrahepatic cholestasis) or outside the liver (extrahepatic cholestasis).
Types of Cholestatic Jaundice
Hepatocellular Jaundice (Intrahepatic Cholestasis)
This type results from the liver’s inability to transport bilirubin into bile canaliculi. The liver cells may be damaged or swollen, making bile movement difficult. Sometimes, the bile canaliculi fail at a cellular level, disrupting bilirubin excretion. Viral hepatitis often causes hepatocellular jaundice.
Obstructive Jaundice (Extrahepatic Cholestasis)
This occurs when bile flow is blocked in the large bile ducts outside the liver. Obstruction prevents bilirubin from entering the bile canaliculi, forcing it back into the bloodstream. As a result, jaundice deepens over time. Gallstones or tumors in the pancreas often cause this condition.
Causes of Cholestatic Jaundice
Intrahepatic Causes
Various liver diseases and conditions can disrupt bile flow. Common intrahepatic causes include:
Viral hepatitis
Autoimmune hepatitis
Postoperative jaundice
Alcoholic hepatitis
Pregnancy-related liver dysfunction
Recurrent idiopathic cholestasis
Primary biliary cirrhosis
Primary sclerosing cholangitis
Certain medications, including oral contraceptives and anabolic steroids
Cirrhosis, regardless of the cause, can also lead to intrahepatic cholestasis due to liver damage affecting bile movement.
Extrahepatic Causes
Blockages outside the liver prevent bile from reaching the intestines. The most common extrahepatic causes include:
Gallstones in the common bile duct
Carcinoma of the pancreas, bile duct, or ampulla
Traumatic biliary stricture
Cystic fibrosis
When bile cannot exit properly, bilirubin builds up, worsening jaundice.
Drugs That Cause Hepatic Cholestasis
Some medications can trigger bile flow disturbances. These include:
Sex hormones
Cyclosporin
Chlorpromazine
Haloperidol
Erythromycin
Cimetidine and ranitidine
Nitrofurantoin
Azathioprine
Imipramine
Oral hypoglycemics
EVALUATION OF JAUNDICE
Evaluation of Jaundice
The first step in evaluating jaundice is determining whether the hyperbilirubinemia originates from a hepatobiliary disease. This can be done by measuring bilirubin levels in the blood. There are two forms: conjugated (direct) and unconjugated (indirect) bilirubin.
In hemolysis, unconjugated bilirubin predominates. This happens because red blood cells break down rapidly, overwhelming the liver’s ability to process bilirubin. Patients with hemolytic anemia often present with symptoms related to excessive red cell destruction.
If conjugated bilirubin is the primary issue, the focus shifts to identifying the underlying cause. It could be due to hepatocellular obstruction following hemolysis or intrahepatic cholestasis. When the liver fails to properly excrete bilirubin into bile, conjugated bilirubin accumulates in the blood.
Diagnosis
The evaluation of jaundice requires a systematic approach. In intrahepatic biliary obstruction, the liver struggles to transport bilirubin efficiently. Extrahepatic obstruction, however, results from a physical blockage in the bile ducts. Proper history-taking, physical examination, and laboratory investigations are essential for an accurate diagnosis.
In some cases, especially in long or short clinical evaluations where investigations are unavailable, doctors rely on differential diagnosis. Age, risk factors, and medical history guide the assessment. By carefully analyzing available data, healthcare professionals can narrow down the possible causes.
History
A thorough patient history is crucial. Doctors should ask about factors that increase the risk of jaundice.
Blood transfusions may suggest prior exposure to infections.
Previous surgeries might indicate postoperative complications leading to bile duct obstruction.
Intravenous drug use and promiscuous sexual activity can increase the likelihood of viral hepatitis.
Alcohol abuse is a major cause of liver damage, leading to alcoholic hepatitis.
Additionally, medication history plays a significant role. Some drugs directly affect liver function.
Medication History
Certain drugs can cause hepatocellular damage or cholestasis. For example:
Chlorpromazine and anabolic steroids affect liver cells, impairing bilirubin processing.
Isoniazid may lead to hepatocellular damage, worsening liver function.
Paracetamol toxicity can result in cholestatic jaundice, where bile flow is obstructed.
Examination of Jaundice
A thorough examination is essential in identifying the cause of jaundice and determining whether it stems from acute or chronic liver disease. Several physical signs provide important clues about underlying conditions.
1. Jaundice
The duration of jaundice helps narrow down its cause. If jaundice lasts less than a month, it is often due to hepatitis. However, if it persists for one to two months, chronic conditions like carcinoma or hepatitis may be responsible. When jaundice gradually deepens, it usually indicates an obstruction due to malignancy.
2. Fever
Fever is a common symptom in viral hepatitis. If fever is accompanied by chills and rigors, cholangitis might be present. This condition often occurs with a gallstone obstructing the bile duct. Patients with cholangitis usually experience three key symptoms: fever, jaundice, and pain in the right upper abdomen.
3. Pruritus (Itching)
Itching varies depending on the cause of jaundice. In viral hepatitis, itching tends to be mild to moderate. However, in obstructive jaundice, it becomes severe due to the accumulation of bile salts in the body. Persistent pruritus may indicate an underlying liver or bile duct problem.
4. Hepatomegaly (Enlarged Liver)
The liver’s texture provides important diagnostic clues. In hepatitis or extrahepatic obstruction, the liver is smooth and tender. In cases of malignancy, it becomes nodular. A careful assessment of liver enlargement helps distinguish between different types of liver diseases.
5. Splenomegaly (Enlarged Spleen)
An enlarged spleen may signal chronic liver disease or portal hypertension. Since the spleen helps regulate blood cells, its enlargement suggests excessive red blood cell breakdown or obstruction in liver circulation.
6. Signs of Chronic Liver Disease
Chronic liver disease presents with several distinctive signs. Clubbing of fingers, palmar erythema (red palms), and anemia are common. Bruising easily occurs due to impaired clotting function. Spider nevi, small red spots resembling spider legs, may appear on the skin. Other signs include ascites (fluid accumulation in the abdomen), gynecomastia (enlarged breast tissue in men), hepatosplenomegaly (simultaneous liver and spleen enlargement), and pitting edema (swelling in the legs).
7. Late Features of Jaundice
Prolonged obstructive jaundice leads to malabsorption due to bile salt deficiency. Over time, patients may experience:
Weight loss due to poor digestion.
Vitamin K deficiency, leading to bleeding problems.
Vitamin D deficiency, causing bone pain.
Steatorrhea, where stools appear greasy due to fat malabsorption.
8. Palpable Gall Bladder
A swollen gall bladder may indicate a serious condition. If the gall bladder is palpable, carcinoma of the gall bladder or pancreas obstructing the bile duct could be the cause. A careful examination helps identify whether the blockage is malignant.
Related questions
What are the different types of jaundice?
How does jaundice develop in the body?
What is the mechanism behind jaundice?
How is jaundice evaluated and diagnosed?
What tests are used to examine jaundice in patients?
9. Stool Changes
Clay-colored stools suggest obstructive jaundice. Normally, bilirubin gives stool its brown color. When bile flow is blocked, stools become pale due to bilirubin deficiency. Stool appearance helps differentiate between different types of jaundice.
10. Urine Changes
Dark urine is a hallmark sign of jaundice. When bilirubin cannot be properly excreted through bile, it enters the bloodstream and passes into the urine. The resulting dark color indicates the presence of conjugated bilirubin, providing crucial diagnostic information.
Investigations
Proper investigations help determine the cause of jaundice and guide effective treatment. Several diagnostic tests measure bilirubin levels and assess liver function, providing valuable insights into the underlying condition.
Liver Function Tests (LFTs)
LFTs evaluate liver health by measuring key enzymes and bilirubin levels. These tests help differentiate between various types of jaundice and detect liver disease. If results show abnormal enzyme levels, it may indicate liver damage or bile flow obstruction.
Serum Bilirubin
Serum bilirubin is an essential test for diagnosing jaundice. It measures bilirubin concentration in the blood and helps classify the type of jaundice.
Hemolytic jaundice leads to a slight increase in bilirubin. The liver processes excess bilirubin efficiently, preventing severe buildup.
Obstructive jaundice results in significantly high bilirubin levels, often exceeding normal limits. This happens primarily due to bile duct blockages, which prevent bilirubin from leaving the liver. As a result, bilirubin accumulates in the bloodstream, gradually causing a deepening yellow discoloration.
Likewise, malignancy-related jaundice also shows high bilirubin levels. In this case, tumors obstruct bile flow, further restricting its movement. Consequently, bilirubin backs up in the blood, progressively leading to severe jaundice and other complications.
Types of Bilirubin Abnormalities
Understanding the type of bilirubin present helps diagnose the specific condition affecting the liver.
Unconjugated bilirubin rises in hemolytic jaundice. Since the liver cannot process bilirubin fast enough, it remains in its unconjugated form.
Conjugated bilirubin increases in obstructive jaundice. Bile flow is blocked, causing bilirubin to build up in the bloodstream.
Mixed bilirubin levels appear in hepatocellular jaundice. Liver cells struggle to process bilirubin effectively, leading to a combination of both forms in the blood.

